A year since assisted suicide became legal, only a small number of physicians are willing to perform the procedure, and their numbers are shrinking. Taking a life is harder than they thought
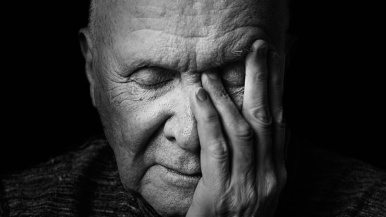
The first thing April Poelstra noticed was the hitch in her father’s shoulder. Jack’s left arm was drooping, hanging limply at his side, as if he didn’t have the muscle to cinch it into alignment. It was the fall of 2015, and Jack was living in Frankville, Ontario, waking up at 4:30 a.m. to plow roads and work odd jobs for a construction company. Jack, then 62, was known to most people in that corner of southern Ontario as J. P. Campbell, the on-air handle he’d used for decades spinning country records at the local radio station. He was handsome, with a rocker’s shag and wry smile, and growing up, April had enjoyed the perks of being the daughter of a small-town celebrity. Her mother had left the family when April was three, leaving Jack to raise her and her two younger sisters, Amber and Alison. In the summer, he would attach their sleds to the riding mower, dragging the squealing kids across the yard. When he was on the air, the girls would crowd around the radio and yell into the speakers, convinced that if they were loud enough he could hear them through the wiring. “Everybody says they have the best dad,” says April, “but I really did.”
Jack tried to downplay his shoulder problems. He visited his doctor for a battery of tests, but always changed the subject when April pressed for details. Over the next few months, she saw her father struggling. During their weekly lunches, he had trouble swallowing. He had a persistent cough. April began searching the Internet for his symptoms, and the more she looked, the more worried she became. In early 2016, her fears were validated: Jack was diagnosed with ALS. Amyotrophic lateral sclerosis, or Lou Gehrig’s disease, attacks the neurons that control the muscles. A person becomes paralyzed in slow motion, losing the ability to walk, to eat, to talk and eventually to breathe, usually within four years. Jack made it clear that he didn’t want to wait that long.
As his body declined, Canada was in the midst of creating legislation that would make it legal to receive a medically assisted death. Jack followed the story obsessively. With his life suddenly circumscribed, the prospect of winning the right to an assisted death became a fixation. Whenever support workers came to the house, he gave them the same line: “Throw some hair on me and bring me to the vet. If I can put down a pet, I shouldn’t need permission for myself.”

In April 2016, four months after his diagnosis, Jack went to the hospital with pneumonia. When he got out two weeks later, he needed a feeding tube and a suction machine for his saliva. He could no longer look after himself, so he moved in with April, her partner, Robert, and their two-year-old daughter, in Smiths Falls, Ontario. The man who had always been a blur of activity suddenly needed his daughter to help him out of bed. The professional smooth talker had trouble speaking, a single sentence sometimes stretching out over excruciating minutes as he struggled for breath. On more than one night, he’d begin to choke, and April would have to call an ambulance to help clear the mucus building up in his throat, watching helplessly as a look of utter horror spread across her father’s face. When she took him to the bathroom each morning, he would say the same thing: “I want to die.”
On June 17, Bill C-14 became law, making medical assistance in dying, or MAID, legal for mentally competent Canadians. Jack Poelstra was overjoyed. His daughter was anxious. She knew it was up to her to get her father what he wanted.
When assisted dying became legal—after decades of activism, years of litigation and months of government debate—the new law pleased almost no one. Unlike the Supreme Court decision, which had made physician-assisted death legal for any competent adult suffering a “grievous and irremediable medical condition,” the government’s bill limits the procedure to people whose death is “reasonably foreseeable.” The law also excludes minors, people suffering from a mental illness and advance directives, which means someone with Alzheimer’s or Huntington’s cannot instruct a physician to end their life at a theoretical point in the future when they are no longer mentally capable. Right-to-die organizations were dismayed that the government had opted for such a narrow interpretation of assisted death. Those opposed to euthanasia were appalled that the decision had been rushed into law.
The bill set out some general rules. In order to receive an assisted death, a person would need to undergo assessments from two doctors or nurse practitioners. Before the procedure, the patient would have to take a 10-day reflection period. Beyond those safeguards, however, doctors were left to navigate this radical change to their profession on their own. No Canadian doctor had ever learned how to perform an assisted death in medical school. There was no Society of Medically Assisted Death to review the literature and come up with best practices. And the questions presented by the law were incredibly complex. How do you perform the procedure? What do you ask patients to determine whether or not they qualify? How do you ensure doctors and nurses get the support they need when they’re suddenly asked to do something that many see as antithetical to their role as healers? And how do you interpret whether a patient’s death is “reasonably foreseeable”—a vague, clinically meaningless phrase that marks the boundary between a medical procedure and a homicide?
During the first year of assisted death in Canada, doctors have had to figure things out for themselves. The process has been an ad hoc, scattershot mess. Policies were hammered out in email chains and over casual conversations. On the west coast, doctors began an informal listserv, which eventually became a new organization, the Canadian Association of MAID Assessors and Providers. The right-to-die advocacy group Dying with Dignity suddenly found themselves in the unfamiliar role of supporting physicians. With 100 patients calling every month, desperately looking for doctors willing to perform assisted deaths, they realized they needed to connect physicians who could mentor one another.

In early 2016, the University Health Network, which includes Toronto General, Toronto Western and Princess Margaret, tried to put together a committee to figure out a policy, but even deciding who would take responsibility for it proved difficult. “Nothing happened for several months until the first requests came in,” says Madeline Li, an oncological psychiatrist at Princess Margaret. Before assisted suicide was legal, she was ambivalent about the procedure, but as she saw UHN struggling, she volunteered to be the person in charge of medically assisted death. “I came to MAID not because I’m a huge advocate for it or because I’m against it, but because it’s now a patient’s right,” says Li. If her hospital was going to provide it, she wanted it to be done correctly.
Building a system for assisted death from scratch, Li found, was a daunting task. To protect doctors who wanted nothing to do with the practice, she created a specific MAID team for UHN: 18 people to do the assessments and 13 to do the procedure itself. When a patient requests a medically assisted death, the front line doctor alerts the team, which takes over the end-of-life process. Two doctors perform the assessments. A third performs the procedure.
Figuring out the best method for death was also complicated. In Oregon, where assisted death is legal, doctors can write patients a prescription for a lethal oral medication and then walk away. Canadian physicians were surprised to learn that the barbiturates used in that protocol weren’t available here. Instead, doctors and nurses deliver a series of drugs intravenously, a process that is far more intimate than writing a prescription. Assisted death, the polite euphemism used to describe the act, is really a misnomer. Doctors don’t “assist” in a death; they are the active agents. “We are doing euthanasia,” says Li. “We are actively ending a life. And it’s very new to us.”
As Li developed a protocol, she realized that assisted death affected everyone in the building—the volunteers and translators, the porters who transport the lethal drugs across floors, the housekeeping staff who could find themselves cleaning a room where person had been killed. At one point, Li was trying to decide whether the medication should come in prefilled syringes or vials. Syringes, she decided, would be more humane, sparing family members the drama of watching a doctor draw the drugs up from a vial. But in order to get prefilled syringes, a pharmacist technician would have to prepare the drugs in a sterile hood, which would add yet another active particpant. As Li discussed the logistical difficulties with the head of pharmacy, they both had a sober moment of realization. In assisted death, of course, sterility was completely unnecessary.
I spoke with one Toronto doctor who asked not to be named. When he received his first request for a medically assisted death shortly after C-14 became law, he couldn’t find a pharmacy willing to prepare the drugs for him. “They all told me, ‘I don’t know, we’ll have to check with corporate policy,’” he says. When he finally found a willing pharmacy, he couldn’t find a nurse that would insert the IV. Despite the fact that he hadn’t started an IV in years, he decided he would do it himself.
His first patient was Gerry Brouwer, a retired school principal living near Uxbridge. Brouwer had progressive supranuclear palsy, a rare brain disorder that produces Parkinson’s-like symptoms. He was an intelligent, independent man who had decided soon after his diagnosis that he did not want to live with a feeding tube. He and his partner of 27 years, Margaret Burrows, had been contemplating a trip to Switzerland for an assisted suicide. The day MAID became legal in Canada, he filed his application.
The doctor and a colleague arrived on July 30 to find Brouwer, Burrows, and some family and friends listening to music. The doctor hadn’t yet learned that it’s best to prepare the medication beforehand, so while the family waited, he spent nearly an hour dealing with paperwork, then taking the drugs out of their boxes and drawing up syringes. He quickly realized that the pharmacy hadn’t given him the entire dose of rocuronium, the final drug of the protocol, which paralyzes the muscles of the body, including the respiratory system, killing the patient.
“We only had a half dose. But even the half dose is practically enough to paralyze a horse,” the doctor says. He told Brouwer that the chances the dose was too small were minuscule, but the choice was his: the doctor could return to the city, pick up some more rocuronium, and drive back, or they could go with what he had. “I trust you,” Brouwer said. The doctor first injected Brouwer with midazolam, a drug used in anaesthesia that puts a patient to sleep. Next came Lidocaine, which numbs the vein. Then propofol, which puts a patient into a deep coma. Finally, he injected the rocuronium. Brouwer was gone within minutes.
The two physicians stayed with Brouwer’s partner for more than two hours, waiting for the coroner to arrive. “It was a calm, incredibly peaceful death,” Burrows says. “I’m grateful that Gerry had the option to have the death he wanted on his terms.”
When April Poelstra set out to find a doctor to end her father’s life, she started with the neurologist treating Jack’s ALS at Hotel Dieu Hospital in Kingston. He was sympathetic, but had no idea how to proceed. The hospital didn’t have a policy yet. He promised he would look into it and get back to her. When April called again a few weeks later, she heard the same thing: “Yes, we support it, but we still don’t have anything in place. I’ll get back to you when we have more information.”
At home, Jack continued to grow thinner and lose motor skills. He was getting impatient, worried that by the time he found a willing doctor, his voice would be gone. His mind was sharp, but people with ALS can experience cognitive dysfunction. Because the law does not allow advance directives, it has created a curious incentive for early action: if a person becomes too sick, he can lose the right to die.
After almost a month, with doctors in Kingston still not responding, April turned to her family physician. Both men had tears in their eyes as Jack told his GP he wanted to die. The doctor was supportive, but said he had no idea how to perform the procedure. He knew a physician in Ottawa, however, that he could ask for a referral.

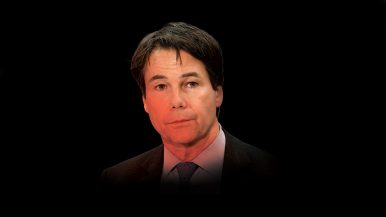
Jack Poelstra’s request made its way to Gerald Ashe, a family doctor and palliative care physician in Brockville, Ontario. Ashe is 66, with an easy charisma and a comfortingly matter-of-fact bedside manner. When he began his medical practice in 1977, talk of assisted suicide was verboten among his colleagues. But over the years it became clear to him that there were times when, for all his effort and expertise, he just couldn’t alleviate a patient’s suffering. In 2014, one of his patients, a 59-year-old father of three with cancer, shot himself. Another man with a terminal illness overdosed on sleeping pills, dying alone without saying goodbye to his wife. Those violent, desperate deaths helped convince Ashe to come out of the closet as a supporter of euthanasia. A few years ago, he joined Dying with Dignity and spoke out publicly about his experiences in palliative care.
When Ashe got on the phone with April Poelstra, he knew it was time to put his words into action. “I always knew it was the right thing to do, but when I spoke to April and heard the plea in her voice about her dad, it was quite sobering,” he explains. He drove up to Smiths Falls for the first assessment in July. There was no official paperwork, so he decided to ask the questions that seemed appropriate. He found Jack shirtless in pyjama bottoms, a feeding tube protruding from his stomach, his granddaughter trundling around the room, climbing onto the couch with him. Ashe listened as Jack explained, his voice faltering, why he no longer wanted to live. “He was a really affable and lovable character,” Ashe remembers. “I knew I had to help him.” It would be his first assisted death.
Ashe is one of only 105 doctors registered in Ontario as willing to perform assisted deaths. While polls show that close to 80 per cent of Canadians believe in the right to assisted death, most doctors remain against it. A Canadian Medical Association survey from 2015 showed 63 per cent of physicians were unwilling to perform the procedure. For them, the question isn’t whether patients should have the option to choose their death. It’s whether doctors should be compelled to kill them.
Of all doctors, palliative care physicians have been the most adamantly against the practice. Dr. David Henderson, president of the Canadian Society of Palliative Care Physicians, says 75 per cent of his members remain opposed. “It goes completely against the philosophy of palliative care,” he says. The purpose of palliative care is to improve a patient’s quality of life without prolonging or hastening their death. Palliative care physicians often see a request for death as a sign of an unmet need—a signal that the doctor just needs to work harder to ease a patient’s physical or psychological distress.

Natalia Novosedlik, a palliative care physician in Toronto, believes part of the reasons for the discrepancy between the public and her profession comes down to familiarity with death. “Having watched many people die, I’m comfortable with the idea that at some point in our life we’re going to need a lot of help from other people,” she says. As a Catholic, Novosedlik feels particularly distraught over the prospect of hastening a patient’s death. In her time working with dying patients, she has watched people find meaning in their final days. “I see a lot of beauty in that,” says Novosedlik. “I see relationships emerging and changing, and I see beauty in caring for another person. For me, that’s kind of a sacred thing. To circumvent that makes me very uncomfortable.”
The law doesn’t force any doctor to perform the procedure, but the College of Physicians and Surgeons of Ontario requires its members make an “effective referral” to a doctor who will. For physicians like Novosedlik, even offering a referral makes them complicit in an immoral act. “It means that I’m initiating a process,” says Novosedlik. When a doctor sends someone to get a CT scan, they do so because they believe a CT scan is medically indicated. But there’s no situation in which Novosedlik believes that death is medically indicated. A group led by the Christian Medical and Dental Society of Canada is bringing the issue to court, seeking a judicial review of the referral policy.
In April, the Ministry of Health and Long-Term Care announced that they were belatedly creating a care co-ordination service that will allow people seeking assisted death to call a central service, bypassing doctors who don’t want to act against their conscience. It’s a necessary tool for navigating an otherwise opaque system. In Canada, Catholic hospitals do not allow the procedure or even assessments within their walls. Even the hospitals that perform MAID, like Mount Sinai and the UHN, do not accept many referrals or actively publicize the service. No institution wants to become known as the place where people go to die.
When most people imagine assisted death, they envision a patient suffering through excruciating pain. The law restricts the practice to cases in which patients are enduring “suffering that is intolerable to them and that cannot be relieved under conditions that they consider acceptable.” To a human being in agony, death is a mercy.
But pain is rarely the reason someone asks to die. In Oregon, where the practice has been legal for 20 years, the most common reasons cited by patients are loss of autonomy, an inability to enjoy life and loss of dignity. Doctors in Ontario say they’ve observed the same reasoning. “It’s a rational decision,” says Madeline Li. “The quality of life is unacceptable.” There is an underlying medical cause, but the suffering is usually existential. Patients find that they are simply playing out the string, without any hope of finding meaning in the limited time available to them.
Writing this article, I spoke with families who described loved ones whose bodies were failing—a slow process in which the abilities that once seemed intrinsic to life fell away, one by one. Gerry Brouwer, an opinionated thinker and eager conversationalist, lost his ability to speak. Colin Ito, a 50-year-old dancer with multiple sclerosis, was no longer able to move his legs, then his arms. Mare Laende, a vivacious 73-year-old woman who had performed as a rhythmic gymnast in the 1968 Olympics, had skin so sensitive she could no longer bear the embrace of her husband of 40 years. When I visited her Toronto Island home just before Christmas, Laende had already been granted the right to an assisted death. Just knowing that she had that option, she said, was a solace. She went through with it a few weeks later, on January 12.
Reports have shown that assisted dying is more common among people who are used to being in control. James Downar, a palliative care physician at UHN and a longtime supporter of assisted suicide, says that the requests he’s seen have come from a particular personality type. “It wouldn’t shock anyone to learn that these are often doctors, lawyers, captains of industry, very successful businesspeople,” says Downar. “These are the people that always get what they want.” Madeline Li has been surprised by how relieved her patients are when they receive permission for a medically assisted death. “It’s the most rapid intervention you can give for end-of-life distress—stronger than any anti-depressant, stronger than any kind of psychological therapy I could have delivered,” she says. For some patients, getting approval for MAID is enough. Of the 32 people assessed at UHN as of April, only 20 had gone through with it.
For some doctors, the aftermath is difficult. Just because doctors are regularly exposed to death doesn’t mean they’re comfortable performing euthanasia. A 2006 study on the emotional effects of physician-assisted death in the Netherlands and Oregon found that doctors often felt isolated and powerless after performing the procedure. At UHN, Li has seen physicians who deal with death on a daily basis break down after conducting a medically assisted death.
Since MAID became legal, the number of willing providers in Ontario has shrunk, as nearly 30 doctors have pulled their names from the ministry’s list. There are a number of possible reasons for this, including the legal risk, however slight, that they could be charged for misinterpreting a new law. Some doctors, though, have simply found themselves overwhelmed by the act of killing another human being. “They thought they were equipped for it, but it was just too difficult,” says Dr. Jeff Blackmer, vice-president of medical professionalism with the Canadian Medical Association. “They lost sleep and they didn’t eat. They worried too much about it.” In the Netherlands, there is a rule of thumb: if a doctor does more than four or five assisted deaths in a year, she’s doing too many. “It’s unnatural, what you’re doing,” says Ruben van Coevorden, a doctor in Amsterdam who has been performing the procedure for 15 years. “You do it for a very good reason, but it’s an exceptional part of medicine. It should not become routine.”
In Ontario, with the majority of doctors thus far unwilling to perform the procedure, assisted death has necessarily become the expertise of a small number of physicians. And with the number of physicians willing to perform assisted deaths shrinking, the burden will increase for the people who remain on the list. As of April, 365 people in Ontario had received a medically assisted death. The family doctor who oversaw the death of Gerry Brouwer has now performed 10 of them. “Just this week I got three referrals,” he told me one day in March. “I don’t know if I can maintain this for another decade, but it’s doable for now.”

On the day of his death, Jack Poelstra woke up and watched Star Trek. A long-time fan, he had binged as much of the show as possible over his final weeks, polishing off the original series, plowing through all of The Next Generation and beginning to work his way through Deep Space Nine. That day, having run out of time, he picked out his favourites from the episodes remaining.
Jack had selected the date, July 27, because it was his father’s birthday. That afternoon, April’s youngest sister, Alison, came to the house to say goodbye. Her father’s death request had been difficult for her to handle. “She wanted nothing to do with any of it,” April says. “She accepted it, but she just couldn’t handle being there.” By 4 p.m., Jack began to get nervous and asked his personal support worker for one of his anxiety medications. Slowly the rest of the family filed in: his daughter Amber, his brother Fred, a family friend, Eddie, who had come down from Brockville to say goodbye. His two-year-old granddaughter gambolled around him, trying to force a plastic cup into his hand for a tea party. When everyone had arrived, he asked April to play some old country songs on her phone. “Well, this is it, that day is here,” singer Jim Reeves crooned. “The day I knew would come, when you would leave me, dear.”
Gerald Ashe arrived at 8 p.m. He asked Jack if he was certain he wanted to die. “Just because I’m here doesn’t mean you have to do this,” Ashe told him. Jack was steadfast. April helped walk her father to his bed. She laid him down, and tucked him in as if he were going to sleep. “You know, I’ll take care of you forever,” she said. “It doesn’t matter: a month, three months, six years, whatever.” He told her he knew, but he wanted to die. “He said he didn’t want to leave us, he was going to miss us, but it had to be done,” she remembers.
April held her father’s left hand, Amber held his right, and their uncle Fred sat at his feet. Ashe injected Jack Poelstra with midazolam, and his eyes closed. His breathing slowed, the rise and fall of his chest barely perceptible. Then Ashe injected him with the Lidocaine and propofol. Jack’s face was pale, his features entirely still, without the slightest flutter beneath his closed eyelids. “He was so at peace,” April remembers. “We knew without a doubt before it was even done, he was no longer there.” Finally Ashe injected him with the rocuronium. “He didn’t even feel the last drug go through,” says April. “I held his hand until everything was done. I didn’t move.”
Since Jack Poelstra, Gerald Ashe has overseen nine more deaths. He’s been there as Canadian families have invented new rituals for a new way of dying—reading poetry and listening to favourite pieces of music, watching as family members have taken turns giving their final hugs and kisses. When I asked Ashe if he was ever upset by the process, if it ever felt like a burden, he thought for a moment. “You know, I think I’m a pretty sensitive guy,” he began. “But I don’t feel upset about it.” The patients had been so sure, so appreciative. The families were so relieved. To Ashe, it was clear that it was something that needed to be done, and he was glad that he was able to do it with care and empathy. “To me it’s one of the most incredible meetings of two human beings,” says Ashe. “If I can meet that person at that time and provide that service? It’s such a privilege. I don’t get upset about it. I sleep well.”
Helping Jack Poelstra die was a poignant experience for Ashe. But it wasn’t sad. Sad was telling a healthy mother with a young family that she had terminal cancer. Sad was walking into the same hospital room of an unconscious patient on life support day after day to talk to the waiting family members, arranged in that modern purgatory of grief. Helping a dying man say goodbye, with his loved ones around him, was moving and solemn, but it was no tragedy. “It was a beautiful thing,” says Ashe of his first death. “It was really, really beautiful.”
Clarification
An earlier version of this story indicated that only 105 doctors in Ontario are willing to perform assisted deaths. As a commenter pointed out, that statistic refers to the number of doctors on the ministry's referral list.