A Life Interrupted: Hassan Rasouli’s journey from an earache to a high-stakes battle over end-of-life decisions
Two years ago, Hassan Rasouli checked into Sunnybrook hospital to have a brain tumour removed, fell into a coma, and provoked a Supreme Court battle over who decides to pull the plug. Then, one day, he awoke

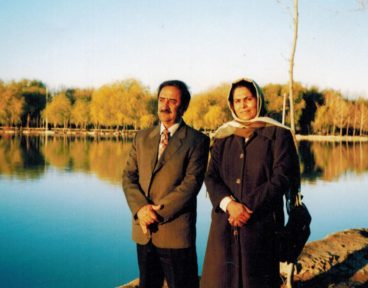
Early in the summer of 2010, Hassan Rasouli, a 59-year-old engineer, had a problem with his right ear. He noticed sounds were coming in muffled and indistinct, as if through a ball of cotton. By August, his hearing loss was getting worse. The ear was slightly numb, too, and at times Rasouli caught himself feeling dizzy. He didn’t think much of it. He had moved from Ishfahan, Iran, to Toronto just four months earlier with his wife, Parichehr Salasel, a family doctor, their 27-year-old daughter, Mojgan, and their 22-year-old son, Mehran. They’d come to Canada with the capacity for risk particular to the new immigrant, the kind that leads someone to abandon a life of familiar comforts for an uncertain world where the possibilities might open up a little wider. They were excited about creating a new life.
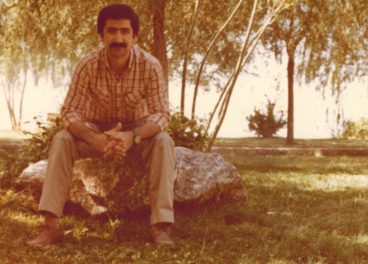
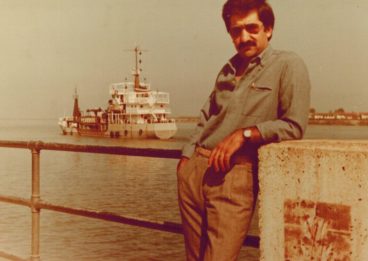
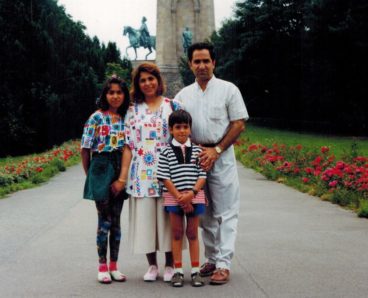
With his bulbous nose, expressive eyebrows, thick moustache and bemused half-smile, Hassan Rasouli looks like a rumpled, Persian Groucho Marx. He was the adventurous one in the family, the parent who would drag the kids on road trips across the country every year, barbecuing kebabs at the roadside and camping in the forests of northern Iran. He was the kind of father who, at family parties, would cajole his embarrassed adolescent daughter into accompanying him on the piano while he sang his favourite pop song.
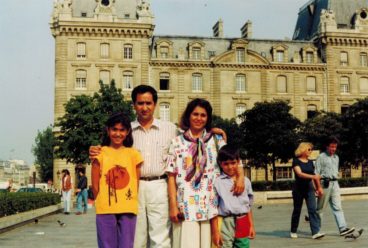
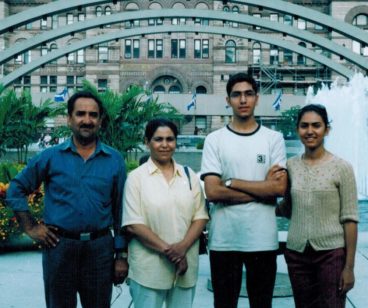
When the Rasoulis qualified for immigration in 2005, Hassan took the family across Canada to find a place to settle down, visiting Montreal, Vancouver and Quebec City before deciding on Toronto, a place where they already had a few friends and relatives and where the work and education opportunities seemed best. They moved into a house near Yonge and Steeles and joined the local mosque. They went on walking tours of Toronto’s parks, exploring their adopted home like tourists. Mojgan signed up at Waterloo to start her second master’s degree, this one in urban planning. Mehran enrolled at the University of Ontario Institute of Technology in Oshawa to study engineering. Salasel was beginning the long process of preparing for Canadian medical exams while Rasouli set up his own engineering consulting company.
At his regular checkup that August, Rasouli told his doctor about the ear problem. He was sent for a CT scan and an MRI, which confirmed Rasouli had a brain tumour. As brain tumours go, it was a good one—it could be removed with a relatively safe, reliable surgery. Rasouli’s doctor recommended Mahmood Fazl, a neurosurgeon at Sunnybrook Health Sciences Centre who happened to have graduated from the same university as Salasel, the best medical school in Iran.
On October 7, the day of the operation, Rasouli was in good spirits. “Don’t worry,” he told Salasel. “I’ll be home in two days.” At noon he said goodbye to Salasel and went into the operating room. Nine hours later, Fazl came down to the waiting room and assured Salasel that the surgery had been a success. They’d managed to remove 99 per cent of the tumour. There had been a small incident when they were intubating Rasouli, Fazl explained, but everything should be fine.
When Salasel visited her husband that evening, however, he was weak and groggy. His breathing was ragged and he had difficulty swallowing. He squeezed Salasel’s hand before shooing her away. That night he went into cardiac arrest. The staff revived him, intubated him and moved him to the critical care unit, where a rotating team of doctors oversaw his care. Over the next few days, Rasouli got worse. He was feeble and agitated. His legs twitched. Salasel remembers one of the doctors trying to reassure her. “She said to me, ‘It’s okay, that’s normal. After brain surgery everyone is like this. Don’t worry, it will get better.’ But it didn’t get better. Every day was worse than the day before.” During a visit on October 15, Rasouli looked weaker than ever. His family gave him a pad of paper. “I am tired,” he scrawled in Persian, the characters falling off the page. They were his last words.
The next day he fell into a coma. He had caught bacterial meningitis after surgery. The bacteria had spread throughout his brain, inflaming his ventricles and setting off a series of strokes. The hospital put Rasouli on a mechanical ventilator. It was an unfortunate situation, the doctors said, but now the family would have to face their new reality: Hassan Rasouli would never regain consciousness.
In the weeks following Rasouli’s surgery, multiple MRIs revealed widespread brain damage. In mid-November, Brian Cuthbertson, the chief of critical care at Sunnybrook, took responsibility for Rasouli’s treatment. He told the family that an escalation of medical care was inappropriate. It was time to let go.
The Rasoulis were stunned. Hassan had been a healthy, vigorous man. He had walked into non-emergency surgery under his own volition and caught a bug from the hospital, and now that same hospital was saying they wanted to let him die? As a practising Shia Muslim, Salasel believed that life was a sacred gift. As a doctor, she thought it was too early to reach such a drastic prognosis. When the doctors suggested cutting off life support, she refused to give her consent. She told them she knew her husband was there, somewhere deep inside. The hospital just needed to give him a chance.
On November 23, the family went to the hospital for another meeting with Cuthbertson, who was accompanied by the hospital’s ethicist, Blair Henry, and a social worker. In the six weeks that Rasouli had been at Sunnybrook, hospital staff had routinely consulted with the family. A neurologist had examined Rasouli on multiple occasions, and each time had concluded that his loss of consciousness was irreversible. The Rasoulis declined the hospital’s offer of an examination by a second neurologist. Now Cuthbertson made it clear that removing Rasouli from the ventilator was the doctors’ unilateral decision. They weren’t asking for consent, they were informing the family: the next day, at 11 a.m., they would be removing Hassan Rasouli from life support.
When Mojgan thinks about that meeting today, she remembers the feeling of confusion and helplessness, of crying on the floor of the hospital. The Rasoulis didn’t know how the country’s legal system worked and had no idea what to do next. That night they called everyone they knew to get advice. One friend spent the morning phoning lawyers. The Rasoulis arrived at Sunnybrook at 9 a.m., terrified that the doctors would try to remove Rasouli’s ventilator before they got there. When the family entered the critical care unit, the curtains around Rasouli’s bed were closed and a paper butterfly was taped to them—the symbol Sunnybrook doctors often use to indicate a patient is going to die. While Mojgan spoke with the hospital’s ethicist in a meeting room, Mehran refused to leave his father’s bedside. He hung verse by the Iranian poet H¯a fez around the bed and stood there, weeping, talking and reading his father’s favourite poems. He was in another world. He guarded the ventilator. When Cuthbertson entered the room, Salasel stood at her husband’s bed and looked him in the eye. “Kill me first, then kill him,” she said.
Cuthbertson relented. He agreed to continue ventilation temporarily, but said there would be no CPR and no new treatment. The hospital suggested the Rasoulis get a lawyer to file an injunction to prevent the termination of care. And with that, Hassan Rasouli’s case turned from a medical fight into a legal one.
The laws in Canada about end-of-life decisions are unclear. There exist well-established precedents for administering treatment: a doctor must first get the permission of the patient or the patient’s substitute decision maker (usually a family member). But on the subject of withdrawing treatment, the courts are divided and the laws are in dispute, mostly because they’re so rarely tested. In the vast majority of disagreements about end-of-life decisions, doctors and the patient’s family are able to reach a consensus without involving lawyers. After a few days of seeing their loved one on life support, some families acquiesce. Or, in many instances, doctors who are eager to avoid a fight submit to a family’s requests, even if they believe the patient is beyond care. A study from 2005 found that 87 per cent of Canadian intensive care medical directors believed that their departments had provided futile care for at least one patient in the previous year. One reason doctors gave for continuing treatment was lack of legal support.
The Rasouli family got in touch with J. Gardner Hodder, a journalist turned lawyer who runs his own small firm out of an office at Adelaide and University. When the family first contacted him, Hodder assumed the Rasouli case would be quickly resolved. In Ontario, when there is an intractable disagreement between a patient’s family and doctors about whether to withdraw life support, the case generally ends up at the Consent and Capacity Board, an independent tribunal created by the province that is usually composed of a psychiatrist, a lawyer and a layperson. The board listens to both sides and comes up with a recommendation, often within a day. “I assumed the Rasouli case would be a matter of sending an associate up to Sunnybrook and saying, ‘Look, if there are disagreements and you don’t think you’re getting the proper consent, let’s go to the Consent and Capacity Board,’ ” says Hodder. Instead, he received a fax from Harry Underwood at McCarthy Tétrault, one of the country’s top law firms, which read, in part: “The critical care physicians at Sunnybrook, for some of whom we act, have determined that they will not continue to offer extraordinary care (mechanical ventilation) to Mr. Rasouli.” The doctors were willing to hold off on removing ventilation as long as the family immediately applied for an injunction. Hodder, who has been in practice for almost 30 years, specializing in business and civil litigation, says he was shocked, but he’d had little experience with the kind of case the Rasoulis were bringing him. Then again, neither had anyone else.
Sunnybrook’s doctors, more than physicians at any other GTA hospital, appear to be aggressively challenging end-of-life laws. In the fall of 2010, around the same time Rasouli was admitted into the hospital, Sunnybrook physicians were before the courts in two other contentious end-of-life cases. The daughter of an 88-year-old World War II veteran named Douglas DeGuerre claimed that doctors chose to ignore his requests for resuscitation, and let him die. She filed a $2.2-million lawsuit that has not yet been settled. Another group of Sunnybrook physicians decided to withhold emergency treatment from Mann Kee Li, a 46-year-old accountant with terminal cancer who had filed a power-of-attorney document explicitly stating he wanted doctors to use any medical measures possible to prolong his life. When Li’s family went to court to try to force the hospital to provide resuscitation, the doctors argued that, despite Li’s wishes, they were not required to provide treatment they believed was outside the standard of care.
“The Sunnybrook doctors have taken the extreme view that it’s their decision alone,” says Mark Handelman, one of Li’s lawyers and the former vice-chair of the Consent and Capacity Board. In the Rasouli case, the doctors are making that same argument again.
“To me it’s obvious that they want to set a precedent that if a physician wants to discontinue treatment he doesn’t need anyone’s say-so,” says Hodder. “They’re looking to settle up a point of law.” The doctors involved in Rasouli’s case declined to speak for this story, as did their lawyer or anyone else
from Sunnybrook.
In January 2011, Hodder applied to the Superior Court of Justice for an injunction to prevent Rasouli’s critical care physicians from removing life support without the consent of Salasel. Hodder argued that the doctors should have brought the case to the Consent and Capacity Board. Under the 1996 Health Care Consent Act, doctors must get permission before administering treatment, and according to Hodder’s argument, “treatment” includes the withdrawal of life support.
The doctors saw things differently. Echoing their argument in the Mann Kee Li case, they said that, in accordance with common law, doctors have no obligation to continue futile treatment simply because a patient demands it. Physicians can choose to ask a patient’s family for their consent and can even go to the Consent and Capacity Board to request it, but doing so is optional. They argued that continuing to treat Hassan Rasouli provided no medical benefit. A family couldn’t demand a ventilator for a hopelessly vegetative patient any more than they could demand antibiotics for someone with a viral infection—it just wouldn’t work, and it was a doctor’s duty to say no.
In March 2011, the Superior Court of Ontario ruled in favour of the Rasouli family. “It is clear from the evidence that the hospital, doctors and substitute decision maker in this case all have as their priority the best interests of the applicant,” Madam Justice Susan Himel wrote in her decision. She believed, however, that the Rasouli case should have been referred to the Consent and Capacity Board. The doctors brought their case to the Ontario Court of Appeal, which also ruled for the family, so the doctors appealed again. This month, the case will be heard at the Supreme Court.
This is the first time such an end-of-life case will go all the way to the Supreme Court in Canada. They rarely reach the upper courts in any country: in most instances, the patient dies before the case can be heard.
Keeping someone like Hassan Rasouli alive for a single day requires a small army. Every morning, doctors, nurses, a physiotherapist, a pharmacist and an occupational therapist all gather at the foot of Rasouli’s bed to discuss his issues. The problems with ICU patients are so severe that each specially trained critical care nurse is responsible for just one or two patients. Every hour, a nurse checks Rasouli’s vital signs—not just his blood pressure and respiratory rate, but also his neurological state and his sputum and urine output. His nurse cleans him up, emptying his catheter bag, sponging him off, shifting his frail body from side to side to prevent bedsores. A critical care physician observes him closely. A respiratory technician checks his ventilator. A pharmacist monitors his dosage, perhaps altering the medication used to stave off infection. In the afternoon, the entire team meets up again to try to figure out how to keep him alive another night.
There are 70 beds in Sunnybrook’s critical care unit, and they are nearly always all occupied. According to a survey published in the Canadian Journal of Anesthesia in 2009, across Ontario there were just over 1,000 critical care beds that could provide mechanical ventilation. A single night in the ICU costs approximately $2,500. A year is nearly $1 million. An ICU bed is a scarce and valuable resource. In a publicly funded system, how we choose to allocate this resource is one of the most difficult questions that policy-makers face.
At every step along the way, the doctors’ lawyer Harry Underwood has been careful to insist that he’s making a legal argument about a patient’s best interests, not about the use of hospital resources. But in the Rasouli case, as in any case about removing a person from life support, the question of resource rationing is present, implicitly, in every argument. “It’s the elephant in the room,” says Arthur Schafer, the director of the Centre for Professional and Applied Ethics at the University of Manitoba. In an affidavit Schafer provided on behalf of the Sunnybrook doctors, he argued that allowing futile care for people like Hassan Rasouli could deny other people much-needed care. “One person’s provision is often another person’s deprivation; so the decision to offer a non-beneficial treatment raises the ethical issue of how to allocate scarce medical resources.”
Medical rationing happens every day, but talking about it is taboo. Officially, there is no room for utilitarianism in the critical care unit. According to the rules of any medical association, the question that must guide a doctor’s actions is “What’s best for the person in front of me?” not “What’s best for the health care system?” or “What’s best for the hospital?” or even “What’s best for all of my patients, as a group?” Unofficially, resource allocation is a serious concern for hospitals and for the health care system as a whole. Sue MacRae, a prominent Toronto-based bioethics consultant who is also a registered nurse, says that medical decisions are often made with limited resources in mind. “It’s rare that a doctor will come out and say, ‘We’re stopping this because it’s costing too much money,’ ” she says. “But I have heard people talk around it. The doctor might say this person is not suitable for ICU care, he’s too sick. And then there’ll be this trailing part of the sentence that says…and this bed is needed for somebody else.”
Three Sunnybrook physicians, including two who have been involved in treating Hassan Rasouli, have made public statements about the doctors’ role in end-of-life decisions before. They wrote at length about critical care medicine in a 2010 issue of the medical journal The Lancet. “Clinicians’ greatest challenge is to engage in decisions about the appropriate extent of life-supporting therapies for patients whose immediate death has been averted, but whose likelihood of returning to a meaningful survival is poor,” they wrote.
They were also frank about the future of critical care units if the current system doesn’t change: “The combination of an aging population and fewer young wage earners in developed countries will create a demand for critical care that cannot be fulfilled as it is presently delivered.”
Rasouli is a harbinger of things to come. According to one study, Ontario will need 57 per cent more ICU beds with mechanical ventilation over the next 20 years. As our population ages and as medical technology improves, giving us the ability to keep critically ill patients alive for years at massive cost, there will be more and more people like Hassan Rasouli.
As the case moved from court to court, the doctors continued to insist that Hassan Rasouli was little more than a vegetable. Throughout this time, however, the family was convinced that Rasouli was in there. “In late December of 2010, I told my father, ‘Please wake up. We miss you,’ ” says Mojgan. Rasouli moved his fingers and the nurses came running. From then on, the family began to notice subtle progress. “In January, he still couldn’t open his eyes,” says Mojgan, “but my mother opened his eyelids for him, and then he kept them open. And through his eyes, his look was familiar to us. He was listening to us and hearing us. He gave us hope that he was there. We got lots of strength from his way of looking.” While the family watched, shadows of Rasouli’s old expressions seemed to play across his face. They believed a raised eyebrow meant he was concentrating. A certain cast to his eye meant he was angry and wanted his kids to leave his bedside and get back to their studies.
It’s common for family members of patients in a vegetative state to see consciousness where it doesn’t exist. “The lay public often pictures vegetative patients as lying there like Sleeping Beauty,” says John Whyte, the director of the Moss Rehabilitation Research Institute in Pennsylvania and an expert in disorders of consciousness. In fact, vegetative patients often move around. They open their eyes and blink. Their hands swim through the air. Their faces flicker through different expressions in a cruel pantomime of conscious life. If a patient moves his eyes often enough, a wife can begin to think she’s being looked at. If his fingers twitch frequently enough, a son can believe his father is trying to communicate.
At Sunnybrook, multiple critical care physicians insisted that Hassan Rasouli’s gestures were pure reflex. The doctors’ court submissions read, “It is clear that Mr. Rasouli’s family loves him very much, and they desperately want to believe that he is conscious and improving. Unfortunately, it is also clear that [their love for him] has coloured their interpretation of his behaviour….It is as certain as anything ever is in medicine that he will never recover any degree of consciousness.”
But Rasouli began exhibiting behaviour that defied that assessment. His wife claimed he could stick out his tongue on command. His eyes seemed to follow his family members around the room. In the summer of 2011, the family recorded video of Rasouli in bed. While Mojgan spoke to him in Farsi, telling him to stick out his fingers, he laboriously flexed them—first giving the thumbs up, then raising his forefinger, then his middle finger.
While lawyers argued for Hassan Rasouli’s life in court, the family was busy learning everything they could about his condition. Salasel poured over his medical records. Mojgan spent hours on the Internet, reading medical reports about people in Rasouli’s situation. They learned that patients in a persistent vegetative state (known as PVS) are notoriously difficult to diagnose. Numerous studies have revealed that up to 43 per cent of patients diagnosed as PVS were in fact minimally conscious. Recently, a study by doctors Adrian Owen and Damian Cruse at Western University revealed that patients who have been diagnosed as PVS under the current criteria might not be as unresponsive as we think. When they put vegetative patients in an EEG helmet that monitors brain activity and asked them to imagine squeezing their hands or wiggling their toes, the brains of 19 per cent of patients responded the same way a conscious person’s brain would. Those bodies lying there—devoid of all the telltale signs by which we infer consciousness—still had minds working feverishly beneath the surface. When the Rasoulis read news reports about the Western University doctors, the family contacted the researchers immediately and arranged to have Hassan Rasouli become part of the next clinical trial.
Last January, neurologists at Sunnybrook announced that they’d reached a new diagnosis. Rasouli wasn’t permanently vegetative, as they had insisted for more than a year. He was now in a minimally conscious state. He could track with his eyes and consistently give the thumbs-up when asked. In his assessment, Sunnybrook neurologist Richard Swartz wrote: “Mr. Rasouli has diffuse and severe limitations of voluntary and reflexive movements of his limbs and eyes, which may limit the range of behavioral responses he can exhibit.” He continued: “He may have more comprehension than he can show.” The examination by Damian Cruse of Western University confirmed the diagnosis.
In the hierarchy of consciousness, being minimally conscious is one step higher than being vegetative and one step below locked-in syndrome, the state in which a patient is fully aware but completely physically incapacitated. “We used to think that neurologic recovery only happened within six months, and if it didn’t happen then you were done,” says the Moss Institute’s John Whyte. It’s becoming increasingly clear that the period of recovery can go on for years, especially for minimally conscious patients. There are mystifying cases like that of Terry Wallis, the man who began talking after lying in a minimally conscious state for 19 years. When doctors examined him, they found his brain had spontaneously rewired itself.
But Wallis is the rarest of exceptions. Far more often, patients linger in a state of uneven consciousness—sometimes able to respond to the people around them, sometimes remaining completely walled off from the outside world. Rasouli is better off than doctors thought he ever would be, but it’s not a grand awakening. “It’s not a coincidence that people used to think that nothing happens after six months,” Whyte says. “Nothing big happens after six months—or it rarely does. Is he likely to go back to work? No. Is he likely to be able to engage in yes-no communication with his family members? Maybe.”
Nevertheless, when the family learned of the new diagnosis, they hoped their legal battle was over. Hodder fought to have the Supreme Court appeal quashed on the basis that the doctors’ argument was predicated on the fact that Rasouli was in a vegetative state. “The withdrawal of life support is not a merciful act applied to somebody with the consciousness of a potato, but rather is the summary execution of a sentient human being,” says Hodder.
The doctors pressed on. Although Rasouli’s diagnosis had changed, the essential legal question had not. Regardless of Rasouli’s state of consciousness, the debate is about who gets to decide. In May, the Supreme Court denied Hodder’s motion to quash the case.
With the Supreme Court set to make a ruling this month, the medical community is hopeful that the judges will lay out some badly needed guidance. A ruling for the doctors could give physicians unprecedented power. If the court decides in the family’s favour, however, it could create a dangerous precedent: patients could demand treatments that doctors believe are unwarranted and even harmful. It’s also possible that doctors worried about being locked into a treatment plan that’s no longer working will take the cautious course and never offer the treatment in the first place.
Because of the rarity of these kinds of cases, the Rasouli decision could have an international impact. Thaddeus Pope, a prominent American commentator on end-of-life issues and the director of the Health Law Institute at Hamline University, has written about the Rasouli case a number of times on his blog. “This could be the most significant judicial examination of medical futility—ever, in the world,” Pope wrote in December 2011.
Advocacy groups that could be affected by the ruling have jumped into the legal proceedings to ensure that their interests are represented. The Euthanasia Prevention Coalition has adopted the Rasouli cause. HIV groups worry about how new legal precedents will affect their members. Mental health advocates, evangelical organizations, associations for critical care nurses and elderly people—they’ve all added their voices to the legal proceedings.
For the family that came to Canada a few years ago, Hassan Rasouli’s journey—from a simple earache to the Supreme Court—has been gut-wrenching and surreal. They’ve watched as a personal tragedy has become a public debate. From his bed, where a ventilator pumps oxygen into his lungs and a feeding tube pushes nutrients into his stomach, Hassan Rasouli has become something both greater and less than a flesh-and-blood person—an abstract cause, and the fulcrum for arguments about the appropriate limits of physicians’ powers, health care rationing, the meaning of medical futility, and even the value of life.
On a Friday evening in August, I accompanied Parichehr Salasel on a visit to her husband at Sunnybrook. In the two years since he was first admitted, his body had shrunken away and he looked small in the bed, surrounded by the whirring and beeping machinery that was keeping him alive.
Rasouli’s eyes were closed when his wife arrived. “Hassan,” Salasel said in a sing-song voice, squeezing his arm. “Hassan, Hassan, Hassan.” His eyes opened. They were oily looking, as if covered in Vaseline, and bloodshot from the medication. Since his strokes, his left eye opens better than his right and his lip curls, Elvis-style. His good eye tracked over to Salasel.
The nurse entered. “How are you, Mrs. Rasouli?” she asked, calling her by her husband’s name.
“Good, good,” Salasel said. She was distracted by something, wiping Rasouli’s forehead, cleaning his eyes, moving with the brisk, confident bedside manner of someone who has spent her life with sick patients. She murmured to her husband in Farsi, kissed his forehead. Salasel and the nurse worked on Rasouli in tandem, sharing the task in a wordless, familiar rhythm. While the nurse cleaned out Rasouli’s mouth with a blue swab, Salasel picked up the slim vacuum wand you find at the dentist’s. “Open, open,” she said in Farsi. She cajoled him some more, and the tiniest gap appeared between Rasouli’s lips. “See?” she said, triumphantly. “He hears me, he opens his mouth.” She sucked the saliva out of his mouth with the implement and kissed his forehead again.
Salasel is there every day. She says if she could live at the hospital, she would. The family has moved from their first house into a smaller place just a few blocks away. They ran out of money about a third of the way through the first trial. Since then, their lawyer has donated hours of his time and the family has started a website to raise funds, so far without much success. Both Mehran and Mojgan are continuing their studies, but once or twice a week they join their mother at the hospital. Salasel talks to her husband, tells him the latest news, exercises him. She looks at him with absolute love, the way you’d want to be looked at if you were Hassan Rasouli.
“Any plans for the holiday weekend, Mrs. Rasouli?” the nurse asked.
“I go to hospital,” Salasel said matter-of-factly. “Every day, hospital. No holiday for me.”
“Well, he had a good day,” the nurse said. She emptied his catheter bag, washed up and left the room. Salasel put a battered tablet computer in Rasouli’s hands and turned on a YouTube video of one of his favourite movies, a black and white Persian version of the story of Samson, the man who lost his strength.
Rasouli’s eyes tracked the room. His hands seemed to clutch the tablet, fingers splayed. These are new gestures for him, tiny alterations in his behaviour that give the family hope. Six months ago he couldn’t sit there, propped up in his hospital bed. He couldn’t grasp the tablet, awkward as it is. The previous two weeks he had been on a home ventilator, a smaller, cheaper machine that could, conceivably, allow him to be transferred out of the Sunnybrook ICU and into another facility.
That’s about as far as the Rasoulis are willing to dream. They know he won’t just stand up, give them a hug and get back to work. Mojgan hopes that one day her father can be more consistently conscious, not talking, not even breathing on his own, but living—looking out the window like he did on rainy days in Iran, feeling the love of his family around him with whatever diminished mental capacities remain. “Right now my father has a life, but another shape than he used to,” says Mojgan. “I should accept that, okay, my father is not able to drive us through all the Canadian provinces, but we can have another style of life
with him.
Maybe he’s not able to sing for me, but I can play those songs from the movies for him.”
Throughout the case, the family has maintained that their disagreement with the hospital has been respectful. The doctors and nurses at Sunnybrook have continued to treat Hassan Rasouli with compassion and professionalism, even as the two sides have battled in court. When he got an infection in the summer, they cured him. When doctors at Western University wanted to examine him, they arranged it. The argument between the family and the doctors comes down to a simple but profound difference of opinion. Ventilation will not cure Hassan Rasouli or repair his brain. For the doctors, continuing treatment provides no medical benefit; it only prolongs a man’s inevitable death and forces him to endure the infections, bedsores, muscle deterioration and other indignities that slowly whittle away at a person whose body is being kept alive by machines. But “no medical benefit” and “futile” are not value-free, objective terms. For the family, the benefit is obvious. A husband and father will continue to live, in however a feeble and compromised state. “His life is not perfect,” says Parichehr Salasel. “His life isn’t good. But he’s there.”
At the hospital, Salasel takes out a package of photos and flips through them in front of her husband. They are photos of Rasouli’s life. There he is, in black and white, as a boy with his parents. There’s Salasel, looking young and beautiful, on the day of their wedding. There’s the entire Rasouli family in 1995, a year they spent in Germany. Then young Mojgan and Mehran in front of the Eiffel Tower, by the famous Zayandeh River in their hometown, at Niagara Falls. And then there they are in Nathan Phillips Square, on the trip when they decided to make Toronto their home, the long reflecting pool stretching out behind them. Every day it’s like this. Hassan Rasouli’s life passes before his eyes, and his wife trusts that he understands what he is seeing.






This is not an argument that happens in other countries- this is a situation entirely unique to Canada, and one which unfortunately could bring into question the entire notion of universal health care. In the USA, the patient would be kept alive for as long as that patient’s HMO would fund the treatment or for as long as the patients family could afford to continue- this is true of most of the world. If this family were asked to pay even a fraction of the costs associated with keeping this man alive, would they? In Canada, these cases are not uncommon unfortunately. No one is saying that this story is not tragic. But really, just because the technical term of persistent vegetative state no long applies- does that mean this patient will ever regain “a meaningful quality of life”. If these cases are allowed to go on- if patients are given the right to demand 88 year old men or a 46 year old man with terminal cancer are to be kept alive indefinitely at an astronomical cost to our health care system, which is already pushed to the limits economically, this is certainly not sustainable! I work in health care, I have seen the misery in the faces of grown men who can’t so much as breath on their own, let alone wipe their own behind- don’t be mistaken, these patients are not kept alive for the benefit of the patients, they are kept alive for the families who just cannot let go.
I absolutely agree with you. I also work in the medical field, and if we asked all doctors working in an Intensive Care Unit, most of us would not want to be resuscitated at all cost.
when does it become treatment or experiment? Yes researcher’s have found something happening but is it really life? If this was done to someone in Germany in 1942 the doctors would have been up on charges. Is it a responsible society that allows this to continue and to allow the “lay person ” to make the decisions about what is futile care? No doctor would ever put the hospital “needs” ahead of the patients needs, as this article seems to hint at .The main question should be not the quantity of life but the Quality of life .Will keeping this gentleman alive improve His quality of life ? or is it just keeping his families idea of quality alive?
Thank you for this insightful article which sheds light on the practices of doctors at Sunnybrook. . I doubt any doctor at Sunnybrook would treat their own family members as they have treated Mr. Rassouli and his family. I guess we now have our own Canadian version of “death panels”.
..I apologize for my poor grammar. In terms of the CT scan, he was admitted with a CT scan, deteriorated over the next several hours, another scan was ordered approximately 10 hours after he arrived, but he was not taken for THAT scan until 2 hours later! Anyone in emergency should be given priority.
The lack of care could happen to anyone – your father, your mother, your sister, your son; at any time, at any hospital. We need to become doctors for our loved ones. It isn’t right.
What an awful tragedy for this family. However, from a medical and ethical standpoint, what is this man’s quality of life? Lying in bed, unable to speak, move– beyond his eyes and hands– or have any meaningful interaction or activities: this sounds to me like hell on earth. Were I in his shoes, I would want to be let go into the great beyond, even if I was minimally conscious. This is not a life. I agree heartily with the previous poster who reflected that these patients are kept alive not for their own benefit, but for that of their poor families who cannot let go.
I think that this family is extremely selfish. There is no quality of life left, while others who could have chance at life are turned away from a much needed bed that he is using and costing a million dollars a year? Not to mention legal costs to take it to the supreme court. It is so wrong, truly disgusting that we are keeping this person alive when there are others that could use the bed and the care. If the family wants him to live, bring him home and pay for care there. If they were actually paying for it maybe they would recognize it is ridiculous to keep him alive. Let Go family. It is time. Give someone a chance who will actually have a quality of life. If this makes me sound mean, then so be it. I am infuriated that this actually goes on in this country – to mirror the statement of another poster, in the USA they would pay for the care as long as they could and then it would end. Deal with it people, enough it enough and it is time to let your father / husband rest in peace. What options would they have back home if they hadn’t moved to Canada?
Anyone who is judging “quality of life” is basing it on their own ablist beliefs. There are people with disabilities who experience life in their own way and are happy to be alive. The I would “rather be this way” cannot make these comments until they themselves are in that actual situation or until it is their child that they are making the decision for. What about the brilliant Stephen Hawking who gradually lost the ability to use his arms, legs and eventually voice. Perhaps the “disability” is not with those who are disabled, but rather with the short coming of the able-bodied…
I was touched by your article very much and would like to help this family. Would you please provide a link on how one can assist this family?
“these patients are not kept alive for the benefit of the patients, they are kept alive for the families who just cannot let go.”— True
My mother had the same situation. We kept paying $1 million RMB to hospital in Beijing. 8 months later, she was still gone. But to the family, she was in hospital, she was still alive. My father talked to her every day in the hospital while she was in a coma. She never woke up ever since she was in hospital that day.
My girl friend had the same brain cancer. She refused to do any operation. She died 2 years ago that year when my mother died.
Ontario already has a system im place to deal with this issue. The doctors caring for Mr. Rasouli refused to apply to the Consent and Capacity Board. They are using Mr. Rasouli in an attempt to change the law. They want to be able to make unilateral life and death decisions without having to obtain lawful consent or worry about being sued. You can bet the doctors are not paying the legal costs!
People are not safe in hospital. Doctors are covertly writing “Do Not Resuscitate” orders in the chart of helpless, trusting patients and the patients are dying.
Doctors know that few families will ever see the chart and their co-workers will not blow the whistle on them. This will only stop after a doctor is charged with manslaughter.
Chanel, I agree with you – based on my experiences of losing my father and the utter lack of care given. People do not understand unless they experience it themselves (which I truly hope they never do).
The Health Care system is broken with many stressed out, over burdened health care professionals still working. Whatever happened to “do no harm” and striving to provide the best quality of life possible.
I also feel saddened for the nurses that have a heart of gold, would do anything for their patients, but are stuck due to the arrogance of “doctor knows best” attitudes.
In regards to Mr. Rasouli. His family never gave up hope on him and rightly so.
Many commenters here talk about the lack of “quality of life”. We are judging people’s worth based on their lack of ability to do what? Contribute to society? Move? Communicate? Many with drug or mental health issues are in the same position. Sometimes it’s a temporary condition with no reliable prognosis. It is an incredibly subjective bar with which to judge the value of a life. More abhorrently, it is *our* view of the value of their life.
As the recent study from Western University suggests, these individuals could very well understand, but are limited in their ability to communicate & respond. I could not conceive of killing or leaving to die someone who understands everything that is going on around them, but because of ‘resource constraints’ decide to let it happen anyway. It’s killing a sentient person because they’re gagged & bound by a medical condition. It’s unconscienable.
“What options would they have back home if they hadn’t moved to Canada?” Madison, please take your uninformed and misguided opinions elsewhere. Iran has both public and private health care systems. The family wouldn’t be left without options, and the same care could likely be arranged in a private hospital.
Now let’s not forget there’s a possibility that “back home” the hospital may have followed procedure more strictly and perhaps prevented the infection in the first place. This article doesn’t really clarify why the infection occurred in the first place (was it just the patient’s immune system or did staff ignore some form of protocol? I doubt the writer would be able to find out anyway).
Doctors in Canada damage their patients and then pretend they are unsalvageable or that their live is unworthy of living and must be killed. It happens in all provinces but Ontario is a leader in this field.
There have been 27 cases brought in front of the Consent and Capacity Board in all, from 2003 till 2012, by doctors who wanted permission to have their patient’s lives terminated by “letting them die”.
In 26 of them, the doctors were given the OK to put their patients to death against their family’s wishes and against their own wishes.
The one exception happened in 2003, at the very beginning of this system, probably by mistake.
In all cases, the people to be killed were 75 or over and in all cases, I have no doubt, most of the patients’ condition that was used as justification to allow the doctors to ask permission of the court to finish them off, was caused directly or indirectly, intentionally or unintentionally, by the very same doctors who had decided not to treat those patients from the get go. I read all the end-of-life decisions of the Board and of every Court. In Rasouli’s case thay had “an incident” diuring the operation and needed to intubate him. That probably came with the dirty tube and the infection they gave him. He did not come ready infected in the Hospital or they would have known about it in pre-op tests.
12 of those cases in the CCB were heard in 2011 and 2012 alone. It is systemic betrayal and deceipt of the population who thinks that their tax dollars ensures their Health Care when they need it most. It looks like healing by killing is becoming pandemic.
Lately they have taken to putting babies to death also. Two such cases ocured in 2012 alone. The state decides who should live and who should die. In the Rasouli case, they gave him meningitis in the Hospital. They caused him the codition he was in when they wanted to off him. It is the way that is available to doctors to erase their own malpractice evidence and to say: “we had permission from the court to do what we did”.
It is stunning. Who gave these judges the permission to decide to have doctors kill their patients? By what authority are they doing this?
A clergyman who a friend of mine arranged to meet with me mentioned this Supreme Court case to me. At this time, My 65-y-o highly intelligent husband is in our local hospital and I am being put under pressure to “pull the plug”. As is commonly the case my husband’s present condition has been adversely affected by “errors of judgement” from medical-staff at 2 of the 4 hospitals he has been moved to. At this time my husband has been ona ventilator for several months but has been succesfully weaned off it twice and then the two above-mantioned “acts” have occured. My husband of 32 years is in ICU in a York Region hospital. He is alert, recognises all visitors by name and beams whenever someone (particlarly the lovely nurses) come to see him Being on a ventilator having had a tracheostomy, he can only whisper –
but can be usually understood together with an alphabet. My husband Loves watching the old movies, I read to him and we have recently started playing board games. At times confused and disorientated – I am advised that this is common for people in long-term ICU care. I am not privy to see what medications my husband is taking but know that pschotropic drugs such as Haldol have been administered.
My husband`s only wish in life is tosee his three grandchildren grow up and in his present condition he is very much able to do so. My wish as his POwer of Attorney for Care is to get Dennis weaned very slowly of the ventilator, get in to West Park for the training to allow him to come home under the care of the 5-mandated trained persons. However to do so, he must be permitted to continue trach-mask trials at a very gradually increasing as-tolerated pace. The RTs say he`s able to do so but the three rotating doctors have decided not to permit this and are pressuring me to remove my beloved husband of the ventilator. It looks as if I am being forced to engage a lawyer to demand the right to live for someone who totaly accepts his current limitations. Yes, I am seeing baby steps of improvement and am working hard to improve his small motor skills at present. This is restricted in part by two fingers having been affected by gangrene after beeing admisinstered a drug to increase his blood-pressure which cuts off the blood circulation to his extremeties. God willing Dennis will continue to improve. This is partially contingent on the 3 rotating Intensivists resuming his slow weaning off the ventilator. There must be many more such cases in Ontario. Much of these issues are due the denial of our very-capable Ontario Ombudsman Andre Marin,to have the Ontario hospital system under his `watch. This is in fact so in other Canadian provinces. Hospital definitely require neutral supervision by our renowned `watch dog` Andre Marin whose large neutral team supervise many other organisations.
Dear Joyce
Please be informed that legally you have a right to demand to be told what medication your husband in on. This is another way of the doctors to opress and supress the families of their targeted victims. They will not disclose the treatment. As his Power of Attorney you have a legal right and by the way, as his wife you have the same legal right and obligation to know exactly what they put him on, for what reason, see alll the test results and ask for a copy of his entire medical Chart so you can take it to a doctor you trust who would inform you if what they are doing is the best treatment to heal him or to kill him. You are by law his substitute decision maker and you have the right and the obligation to give or withhold consent on his behalf. The consent must be informed. THEY HAVE TO DISCLOSE EVERYTHING TO YOU. Too bad if they don’t like it and they usually don’t. You’ll hear every excuse under the sun as to why they cannot provide you with the information you need so get prepared before you go and ask for it. All you’ll hear is excuses, then denial and then hostility and rejection. All Hospitals are trained to gueard against the patients and their families. It’s unwritten policy. If they make trouble, ask to see the written policies regarding disclosure of Patient’s Records to the patient or his substitute decision maker. When you see the Policy, ask them to give you a photocopy. You need to keep parallel records of your own.
For this post
“Chanel, I agree with you – based on my experiences of losing my father and the utter lack of care given. People do not understand unless they experience it themselves (which I truly hope they never do).
The Health Care system is broken with many stressed out, over burdened health care professionals still working. Whatever happened to “do no harm” and striving to provide the best quality of life possible.
I also feel saddened for the nurses that have a heart of gold, would do anything for their patients, but are stuck due to the arrogance of “doctor knows best” attitudes.
In regards to Mr. Rasouli. His family never gave up hope on him and rightly so.””
Nurses actually control most hospitals. A lot of them push for making patients DNR coz that means less work for them, I am sick of all of that and being on break most of the time when at work. Please dont attack the doctors when u dont know enough
It is surprising to me that some of these comments suggest religious reasons to resuscitate dead people. Sometimes it is your time to go. I’ve had patients resuscitated multiple times in the course of a week until eventually a resuscitation fails. It really seems like fighting nature.
In my experience it is typically the opposite of what has been described. Most doctor’s do not want to accept when there is not much they can do for the patient. They suggest further interventions for people who have already had poor outcomes, often very frail elderly people. Doctors are the only ones on our team who can have the patient’s family fill out the DNR form and they seem to avoid that conversation at all cost.
I’m not saying a family should be pressured to sign. I’m saying most are not given the time to have a conversation about it. Also, most are not really aware of what the expected outcome from resuscitation is for their loved one. Many frail, complex patients will need repeated interventions. They are kept in and out of the ICU instead of in a more comfortable environment.
Also, most of the time when I’ve seen a change in the orders occur, it has been from DNR to full code when the patient’s family has assumed the role of decision maker. Sometimes the patient previously expressed desire to be DNR but their family would like them resuscitated.
That is so untrue..I have seen medical doctors withdraw life support on their family members all the time. It is torturous to be on life support…your muscles contract and are so painful, you develop horrible sores, you have horrible spasms as you are trying to cough up secretions that build in your lungs…the list goes on. As a nurse I have seen this time after time. Also the money we are spending on futile medical treatment is being lost to preventative medicine. Now OHIP will only pay for a physical every three years. There could be many missed illness in that time. Let’s use our resources wisely. God bless this family…but they are doing this for them not the patient.