15 thoughts on “Doctors are rebelling against Ontario’s crumbling healthcare system”
Comments are closed.
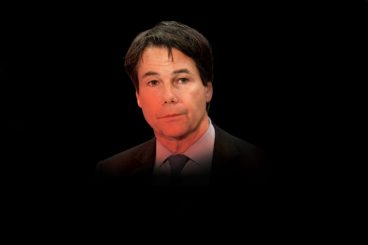
Health Minister Eric Hoskins has locked horns with Ontario’s physicians. His government is out of cash. The overworked doctors are protecting their paycheques. And neither side will budge. Inside the bloodthirsty battles over the province’s health care
When Eric Hoskins took over as Ontario’s minister of health in June 2014, he walked right into a fight. The day he started on the job, his new ministry was already embroiled in failing contract negotiations with the Ontario Medical Association, which represents the province’s more than 28,000 practising physicians. Hoskins was the long-standing MPP from the midtown Toronto riding of St. Paul’s, with a PhD from Oxford and a history of humanitarian work in some of the world’s most war-ravaged regions. He was also a doctor himself. He seemed like the ideal person to broker a new peace.
The key issue was the money that was being spent on physicians. Doctors’ billings had surged over the past decade, and in 2013, OHIP had paid them a total of $11.4 billion, the single largest line item in the provincial budget. One of every four dollars spent on Ontario health care was going to doctors. Hoskins’ marching orders were clear and simple: keep a lid on it. He needed to improve the system without increasing costs, and that meant paying physicians less—in some cases, a lot less.
Five months after Hoskins became health minister, still with no agreement in sight, the two sides appointed former Ontario chief justice Warren Winkler as their conciliator. Winkler surveyed the situation and quickly realized it was a dumpster fire. The government wanted to cap the amount it would pay its physicians at roughly $11.4 billion, with a small annual increase. The OMA was concerned about the effects of Ontario’s ballooning aging population and the fact that, with up to 700 more doctors joining its ranks every year, that money would be spread ever thinner.
These positions, Winkler later wrote in his final report, were “irreconcilable.” Forebodingly, he concluded that “absent some rationalization, the system may not be sustainable.” He told both sides that, unless they overhauled how health care is delivered, the day would soon come when they would never be able to get a deal again. Both parties agreed that his doomsday assessment was correct.
When the province tabled its final offer on December 11, the OMA balked. Winkler told them that the deal was as good as they were going to get. The OMA refused to reconsider—and Hoskins went on the offensive. He imposed that final offer unilaterally, which capped physician payments at $11.4 billion. A few months later, when billings busted through the cap, Hoskins started clawing back doctors’ earnings. All physicians in Ontario now have 4.45 per cent of their income withheld from their monthly OHIP cheques. The government keeps that money, forever, in its efforts to balance its budget.
Many physicians believed the Liberals were charging them a “doctor tax” and using it to pay for billion-dollar gas plant and eHealth scandals. In 2016, after trying for more than 15 months to get the OMA back to the bargaining table, Hoskins changed his tactic. At a press conference in April, he declared that Ontario’s doctors, with average billings of $368,000 per year, were among the highest-paid in Canada. A total of 506 physicians invoiced OHIP for more than $1 million in 2014, and three types of specialists made up more than half of them: radiologists, ophthalmologists and cardiologists. If Hoskins could not cajole the OMA back to the table, he’d shame them back.
No doctor was more sensitive to the negotiating position than Virginia Walley, the OMA’s president. Walley, a pathologist by training, has been a teacher, a department chief and a hospital administrator, so she understood the government’s concern about rising health care costs. But she wasn’t inclined to let the government unilaterally decide doctors’ future without input from doctors themselves.
So she sat down with the devil. During a few days in late May, the OMA and the ministry hammered out a four-year contract. The discussions began secretively, with official negotiating teams called in only midway through, when the broad strokes of a deal were already in place. When Hoskins and Walley announced they’d reached a tentative agreement on July 11, the news came as a surprise.
The details, at first glance, were scandalous to many OMA members. Walley agreed to abide by a cap of $11.9 billion on total OHIP billings. The earnings clawback would remain in place. While the deal included a 2.5 per cent annual increase to the cap, both parties agreed that most of those new funds would be eaten up by new doctors entering practice and aging patients needing more care. In other words, the deal would likely amount, at best, to a pay freeze for four years. The one upside for the doctors was that the deal enshrined the OMA as “co-managers” of the health care system, which meant that the government would no longer be able to make budget decisions without them. Hoskins would have to work with the doctors on every change.
The day after the deal was announced, Concerned Ontario Doctors, a Facebook group with 20,000 members, launched the Twitter hashtag #IVoteNo. The next week, the group called for the resignations of Hoskins, deputy health minister Bob Bell and Walley, as well as the OMA board of directors and its negotiating team. The #IVoteNo hashtag exploded with comments, ranging from reasoned debate to pure histrionics. “I remember when I used to trust OMA implicitly,” tweeted Nadia Alam, one of the founders of Concerned Ontario Doctors and its most prolific tweeter. “I used to trust Govt’s benevolence. Now I question both.”
In the end, 63 per cent of the province’s physicians voted against the deal, overwhelmingly rejecting Hoskins’ and Walley’s gambit. They claimed they were defending the best interest of patients. If this were truly about patients, it would have been settled long ago.

The way Ontario pays its doctors is utterly anachronistic. It goes all the way back to Tommy Douglas and the founding of Canadian medicare. Back then, doctors didn’t want to become salaried government employees. Instead, they accepted the role of independent contractors who bill the ministry for their services. In Ontario, physicians track every procedure and consultation they perform, and send a detailed invoice to OHIP every month, which for the average Ontario doctor is for just over $30,000. From those funds they pay the salaries of their secretaries and assistants, their office rent and utilities, business taxes, and all other expenses—typically around $13,000 or so. They keep the rest for themselves.
This system, known as fee-for-service, preserves physician independence. Doctors decide what care the patient needs and the government doesn’t ask questions. But in the past few years, the fee-for-service system has become unwieldy and voraciously expensive. The OHIP schedule of benefits, which lists fee rates for the services doctors perform, is bloated beyond utility. As new medical procedures emerge—in-vitro fertilization, for instance—OHIP adds new codes to the schedule but rarely removes any old ones. There are now more than 7,300 different codes in the schedule of benefits, some of which haven’t been used in a decade or more. Alberta, by contrast, lists just 3,200 codes in its schedule of benefits.
Other procedures don’t even make it into the OHIP fee schedule. I spoke to Ian McGilvray, a Toronto General Hospital hepatobiliary surgeon and one of the few doctors in the world who have successfully removed a section of the vena cava, the large vein that carries blood back to the heart. “There is nothing in the fee schedule for a caval reconstruction,” McGilvray explains. “So I’ll bill for an arterial reconstruction, and it will be denied.” Then he negotiates with OHIP to sort out a fee, a process that can take months to resolve—and if they can’t resolve it within a year, McGilvray’s claim expires and he is left unpaid. At one point, OHIP owed him hundreds of thousands of dollars. “OHIP will often substitute a less expensive fee code than the one I’ve claimed and pay me for that,” he says. “It’s wildly complicated. I’ve burnt out five secretaries trying to figure it out.” He now has a billing agent whose job is to handle his OHIP filings for him.
The biggest problem with the fee-for-service system is the fact that we can’t afford the number of procedures doctors perform. Ontario’s population is growing by more than 160,000 people per year. It’s also aging. Last year there were 2.2 million seniors over age 65 in Ontario. Their ranks are projected to swell by more than 100,000 per year for the next 15 years. And the burden they place on the health care system is growing exponentially. The average 40-year-old costs the system $2,290 per year. An average 65-year-old, meanwhile, costs $6,298; a 75-year-old costs $11,557; and an 85-year-old costs $24,387.
Both the Ministry of Health and the OMA have long known that OHIP will buckle under the pressure of the aging population. Yet they’ve been unable to reorganize the system to deal with it. The province will need better support for home care, and more chronic care and mental health physicians. And that’s one reason why Eric Hoskins curbed doctor billing.
From a budgetary perspective, the clawback makes sense. From the perspective of individual physicians, it’s much harder to reconcile. My wife, Lynn, is a general surgeon in Peterborough. She performs a variety of procedures, including appendectomies, gall bladder removals, colonoscopies and lots of cancer surgeries: breast lumpectomies and mastectomies, and colon resections. Her clinical work involves counselling patients through the intensely emotional path toward surgical intervention. She assesses them, devises a plan for their care and then executes it, co-ordinating with radiologists and anesthesiologists and oncologists and family doctors and nurses and hospital administrators.
In addition to her work in the clinic and the OR, every sixth night Lynn is on call—available to examine any patient who shows up in the emergency ward with a condition that might require surgery. During these nights I notice the growing medical needs of baby boomers. Five years ago, when Lynn first started practice, there were often nights on call when no patients would show up, when we’d stay home and binge-watch episodes of The Wire and her phone would not ring. That never happens anymore. Time on call is now spent mostly at the hospital. Amid the emergency appendectomies, the breast cancer lumpectomies and the aging-boomer colon surgeries, the work is relentless and exhausting.
As a result of the clawbacks, Lynn is paid less every year for every procedure she performs. We try to look at it from a business perspective: her revenues are down four per cent. It happens to all small firms, and for now it’s manageable. But when other businesses are faced with a drop in revenues, it’s usually because they’ve lost customers. Not so for doctors; the ailing patients just keep coming. Lynn responds by trying to see more of them: extending her clinic days with extra appointments and asking the hospital for additional time in the OR. Partly it’s to make up the revenue shortfall, because there are annual cost increases on her lease and utilities, and raises to pay her staff. Mostly it’s because the demand for her services is endless: there are too many people with cancer who need surgery.
The more patients she sees, and the more patients all her colleagues see, the more they bill to OHIP. The more they bill OHIP, the more they risk exceeding the cap on physician payments. And if they bust through the cap again—which is entirely likely—the province will increase the clawback and reduce their earnings again. The system has gone haywire. Overtime is supposed to be paid at a premium, not at a discount.
The crumbling system is taking a heavy toll on physician morale. Concerned Ontario Doctors claims that, as medical practice becomes too onerous, older physicians are retiring and others in mid-career are moving elsewhere to practice. None of this worries Hoskins or the ministry: for years now, Ontario has had a glut of recently graduated, underemployed physicians, and they are happy to fill the void. They are the only happy doctors in Ontario right now.
Eric Hoskins is a doctor by training, but medicine was never his true calling. After receiving his MD from McMaster, he ended up in Sudan in the late 1980s, working at the University of Khartoum’s School of Medicine. “I was the only white guy out of a student population of 25,000,” he recalls. Hoskins witnessed the military coup d’état that installed the brutal Islamist regime of General Omar al-Bashir. When the med students protested the dictatorship, al-Bashir’s men arrested dozens of them, including Hoskins’ officemate. His lifeless body was returned a week later, with his fingernails pulled out and burn marks on the corpse.
Watching such horrors gave him a stoic character, which serves him well in his dealings with outraged physicians. Hoskins is the most hated doctor in Ontario. When he was appointed health minister, a rumour immediately circulated about him in hospital hallways—and persists to this day—that he’s never practised a day of medicine in Ontario. When I asked him about it, he debunked the myth: since the 1990s, Hoskins has practised part-time at a family clinic in Toronto that serves east African refugees and immigrants. (He still does occasional shifts there without charging OHIP, to avoid any conflict of interest.)
He says he sympathizes with the physicians—his wife, Samantha Nutt, is on staff at Women’s College Hospital—but his job is to defend the interests of taxpayers, who want a publicly funded health care system but can’t afford its runaway costs. And from a big-picture perspective, what he’s asking doctors to do isn’t that bad. Every comparative ranking of health care systems rates Canada among the worst in the developed world. One recent study by the Commonwealth Fund listed Canada second-last among 11 wealthy nations. It beat out only the United States, and got low marks for timeliness of care, safety and efficiency.
The fact that doctors bill more than $11 billion annually makes them something like a corporation—their revenues are roughly the same as Air Canada’s or Canadian Tire’s. When companies of that size have to deal with revenue freezes or shortfalls, they respond by finding efficiencies, eliminating duplication and waste, lowering wages or prices, squeezing suppliers for discounts. They take a hard look at how they run their business, and they usually become better companies as a result. Doctors refuse to do this work. Hoskins is determined to force them.
He has made it clear that only some doctors are overpaid, and that it’s time to update the fee codes to rebalance things. Among physicians, this disparity is called “relativity,” and it has grown out of proportion as a result of technological advances. Some medical images used to require extensive study to reach a diagnosis. Today, software can take those images and construct a three-dimensional model of your innards in minutes, and radiologists can read them from home on their computers. The work is much faster than it used to be and has become disproportionately lucrative.
Twenty years ago, cataract surgery took a full hour to complete. Now it takes 20 minutes. The OHIP fee code values the procedure at $397.50, which means that ophthalmologists can earn $1,000 per hour. Meanwhile, as one emergency room physician told me, “If you come into the ER dead and I resuscitate you, that takes as much time as cataract surgery, and I get $70.”
Every doctor knows relativity is a problem, but they cannot find a way to fix it because the wealthiest specialties, which hold a lot of sway within the OMA, will always aggressively defend their sweet deal. The last time the OMA agreed to curb relativity, in the late ’90s, in part by capping a number of radiologist fees, they were sued by the Ontario Association of Radiologists, who tried, unsuccessfully, to break away completely from OMA representation.
Another way to save money is to eliminate unnecessary treatments and procedures. Patients aren’t supposed to get every X-ray, CT scan, MRI or minor surgery they think they’re entitled to based on their WebMD search. Their doctor is supposed to decide what’s appropriate. There are hundreds of procedures that doctors routinely do but shouldn’t. There’s no point in ordering screening chest X-rays and ECGs for patients at low risk of heart disease; in fact, a false positive on such a test can lead to additional unnecessary procedures for arterial stents. Depending on a patient’s age, surgery to repair a torn meniscus in the knee actually does nothing to alleviate pain, yet the procedure is still performed.
When I spoke to Hoskins, he raised the example of methadone treatment. Some doctors who prescribe the drug bill OHIP for their patients’ urine tests, which are used to make sure they are taking their dose. “It’s a urine dipstick test that I could teach you to do in 14 seconds,” says Hoskins. There are two dozen methadone-prescribing doctors in Ontario, who billed OHIP for over $1 million last year, and they derive most of their income from that test. Methadone is both overcompensated and overprescribed in Ontario, costing OHIP more than $150 million annually.
By and large, doctors don’t do unnecessary procedures to bilk the system. They order the extra X-rays to make sure they haven’t missed anything; they do the knee surgery because the patient is in pain; they prescribe the methadone so an addict doesn’t relapse. That doesn’t make it any cheaper. Researchers are only just beginning to quantify the cost of inappropriate care, but a 2012 study by the Dartmouth Institute for Health Policy and Clinical Practice found that 30 per cent of all procedures ordered by physicians are wasteful.
The government is unwilling to decide what kind of pay cut some specialists should get, nor will it decide alone which procedures it won’t pay for anymore—and nor should it. Doctors need to make those calls, because they are the care experts. Certainly no doctor wants bureaucrats making these decisions for them. The U.S. tried that back in the 1990s, when insurance companies started telling doctors what they could and couldn’t do for patients, and it provoked a flood of anger, frustration and resentment from all involved.
In Alberta, the Health Ministry and the Alberta Medical Association have formed a committee that has begun to tackle such spending issues. Last month it reduced some radiologist and ophthalmologist fees by more than 20 per cent. Here in Ontario, the deal the OMA and Hoskins negotiated this summer would have committed doctors to a similar process.
In the aftermath of the deal’s failure, the government’s position hasn’t changed. Health care is still broken. In a written statement released after the results of the vote, Hoskins said, “Going forward, the government will be guided by the need to secure a stable and predictable budget.” Read his lips: he is going to keep capping doctors’ payments and clawing back their earnings until they come around.
The rift in Ontario’s medical community boils down to a simple question: are doctors still stewards of the health care system, or are they just a higher-paid class of rank-and-file employee? The OMA traditionally projects the image of doctors as leaders. Because they know what’s best for patients, they also have special insight on how to organize and manage everything else—clinics and hospitals and support staff and supplies and equipment.
This is the view of Virginia Walley, who insists her organization isn’t a union. Walley is soft-spoken and even-keeled, and articulates a clear view of what she thinks her profession must be. “The trust we are given by patients and the public comes with broader responsibility for the system,” she says.
Her traditional view of the profession is no longer the prevailing one. Last year, when Queen’s Park and the OMA were trying to get back to the bargaining table, the OMA asked the government to grant binding arbitration. They argued that, because doctors cannot strike, they wanted to defer to a neutral arbitrator, and both sides would have to abide by the arbitrator’s ruling. The government’s answer came swiftly and decisively: no. In response, the OMA launched a court challenge and made their position clear. Until they have binding arbitration, they won’t discuss anything else.
From the government’s perspective, binding arbitration would be a financial disaster. It is the same mechanism that has, over the last decade, granted monstrous pay increases to police and firefighters while also making it impossible to reform those services. And unlike police officers or firefighters or nurses, doctors set their own work hours. If an arbitrator awarded physicians a large pay increase, and doctors responded by increasing the number of patients they saw, they’d bankrupt the province. It nearly happened in British Columbia: back in 2002, an arbitrator there granted doctors a 20 per cent fee increase. The government promptly passed legislation to invalidate the ruling.
The demand for binding arbitration signals a deep transformation within the profession. Doctors think they’re being shafted by the man and want court protection from abuse of power. When they ask for binding arbitration, and when they refuse to discuss anything else until they get it, they are abdicating their role as stewards of the system. They no longer see themselves as management but as labour.
Walley has insisted, over and over, that most doctors want to be system leaders. The results of August’s vote do not support her claim. Of the province’s 28,000 practising physicians, there are plenty—probably a majority—whose sole ambition is to be good front-line caregivers. That is as noble an ambition as any other. Even patients don’t need their doctors to be leaders. They just need them to be good doctors.
The trouble is that, right now, governments and taxpayers need their doctors to be more. The OMA may not survive the infighting between the system-leader collaborationists and the arbitration-or-bust hardliners. Even Walley, who so willingly negotiated with the province, now says that arbitration should come before any other talks.
The OMA has a split personality and might actually be better off as two separate organizations: a union to negotiate the contracts and play politics, and a professional association of physician leaders who are interested in reforming the health care system. In late August, Hoskins even conceded that he’d be open to recognizing the OMA as a union—although that would mean they’d have to disclose their salaries and relinquish the right to incorporate.
While we all wait for the OMA to sort itself out, the budget continues to buckle. Doctors can blame the ministry all they want for underfunding it, but no government can fund an antiquated and ballooning system forever. Even Ottawa is getting involved: the feds have suggested that health care needs an overhaul, and they will not give the provinces more money if it will only be used to pay for doctors’ compensation. Health care needs fixing, and the question is who will lead the fix. If the OMA stalls the reform process for years, they may get much more than they bargained for.
Comments are closed.
Love this article: Kudos for being so balance and not succumbing to bias despite having a spouse as a surgeon.
At 750k for radiologists. I think 4 percent cutback is reasonable.
All doctors have received a greater than 4% cut, not just radiologists. Most of us make a small fraction of that figure. Unfortunately, just cutting the fees of high billing physicians does not make a big enough impact on the budget.
I voted in favour of the OMA/government agreement, even though it would have inevitably meant more fee cuts. I thought it was a better alternative for the profession and the health care system than having no agreement. However, I lost trust in the OMA, because of the poor, and at times, misleading communication with members. It would have been a much easier choice to make if we felt we were getting transparent advice from our representatives. On top of this the government ran a disingenuous PR campaign against physicians. All of these factors made the proposed agreement less credible.
This article ignores a third and very real pressure on the system: uncontrolled and unaccountable patient demand. When a patient can doctor-shop multiple times for the same problem until they get what they want, with no consequence on resource consumption, then the system is sucked dry. No politician wants to acknowledge this difficult truth, since addressing accountability for inappropriate use by patients (growing in number, age and need) is politically unattractive and costs votes. The unspoken reality is that the vast majority of healthcare demand is driven by patients, not gov’t or physicians. Since the govt doesn’t want to hold patients accountable, they want to shift the blame on increasing costs on doctors who are required to provide services by the CPSO, and forced to bill OHIP for these services (since extra billing was banned in the 1990s). So as a physician, when you are forced to work to provide services that patients demand (but may not need), and must bill the govt for those services (as you’re not allowed to bill anyone else), then of course the system pressures will build. Scapegoating physicians in Ontario for growing needs/costs will never work, and physicians can never agree to pay for a growing misfunded system that has endless demand and limited resources. Physicians do not have the power to control demand of services overall, nor should they have to pay for growing sources above some budget cap created by a govt that has failed to control its spending elsewhere…Physicians should and would gladly participate in health care reform and innovation, but should never agree to pay for ongoing failures to fund current care models appropriately…
Thankyou for a incisive, balanced and accurate article. Your description of this chronic view, that the healthcare services group is acting more as a union that a business is the absolute truth – in fact I would count them as the highest paid union membership in the entire world. Fact check what average radiologists, for instance, receive in compensation in other G7 countries against their eduction costs and Canada by far provides the most.
On this topic of Radiologists and other specialties – not only does the government highly subsidize all doctors education, they also receive some of the highest wages for a social system in the world without comparable performance benchmarks to meet. While family doctors are unfairly compensated for their work – particularly when considering their business costs such as office management, facilities and such – what I have yet to see with the medical specialties is a true overview of what a *great* deal they have. To summarize – the taxpayers subside your medical training costs which last 7 years at minimum (most residents have a 5 year program and receive 55-75k+ per year in salary as ‘students’ while they are training). Additionally once working and earning fees as specialist – which if family and other doctors were excludes would likely average 500k per year or higher – taxpayers pay hospital facility fees, operations staff, nursing, equipment capital costs and so on. Radiologists utilize these facilities without paying the true proportional overhead of these costs. Additionally, radiologists and other specialties have naturally received incredible productivity improvements through the system making purchases over time for CAT/MRI and other imaging technologies without a proportional reduction in fees.
Finally, and this is the only point that is important that was not discussed – above inflation pay increases with tax revenue increases at inflation. A crude illustration is that, as a whole, fees have generally increased at *greater than inflation* for over 10 years. If inflation tracks at 1.5% annually over the past 10 years, and doctors have received 5% (some stats show it has exceeded 6%), in order for the tax payers to catch up in producing taxes to cover the gap even if we assumed inflation increased today to 3%, doctor pay would have to be ‘frozen’ for the next 10 years to simply begin affording the system pay structure as it stands today.
Business keeps such imbalances in check through competition. Unions prevent such. Ontario physicians are playing both sides – bargaining as a union, while operating as a business.
Time to pick. Taxpayers require you to.
Are there any numbers on people who doctor-shop and the costs associated with that?
Great article and things boil down to this. Arbitrary price-fixing distorts the market. The government should walk away and patients and doctors need to sort out supply and demand through normal price discovery.
Medicare and Obamacare in the US has us experiencing the same dynamics.
Just ask your parents and friends, You will find with a very small group the number is high, especially in US and Medicare. Disclosure, I am an Internist, father, husband, patient, son and son-in-law.
Socialist economics never work. Price fixing by the monopsony artificially cause price to falsely drop. This article highlights this reality. Open hostilities historically follow.
There are few regular tracking mechanisms for routine multiple visits from the same patient for the same problem in a short time frame, mostly because OHIP/MOHLTC is not interested in tracking this…in our ER, we do track frequent flyers and our hospital administrators try to implement care paths to intercept them before coming to the ED for their daily (or more) visits…Sometimes the numbers are so high, however, that the police investigate these behaviours and rightfully charge them with mischief for abuse of resources…for example, one of our FFs was charged and jailed for a week (thankfully) for calling ambulances 105 times in 2 months (almost twice a day) for non urgent problems, rides downtown, etc. Of course, they never pay their ambulance bills as most are on social assistance or some other excuse, so taxpayers keep footing these expensive bills and reduce resources for the rest of the population…Every ER in Ontario has these numbers, but politicians won’t do anything about this as it costs them bad publicity and votes…
Canada would benefit from Advance Practice Providers i.e. -Nurse Practitioners and Physician Assistants. We do all the same things as Doctors for less than half the pay. This could be addressed in Canada. I see patients, interpret data, order tests, write orders, consult, write electronic prescriptions (and yes i can write for any drug here in the US), talk to families and so on.
I am a Canadian working in the US. I tried to obtain my NP license in Canada but after almost 1 thousand dollars and 18 months of forms, tests and phone calls, I was denied. My 4 year masters degree at the University of Rochester is not good enough.
Mid Level providers are at every level of health care in the US.
This article is pretty well balanced and the best of any written I’ve read on this issue so far. Thank you Toronto Life.
Suneel – I think your point is bang on as well. There is no political will to deal with the patient demand side so it’s unfair to expect that Doctors shoulder the brunt of expenses.
I work with primary care physicians so I am privy to the gross inefficiencies of our healthcare system. I do not believe it will ever improve without a complete system overhaul. Here is a great HBR Michael Porter podcast that I recently listened to which starts to address this very issue: https://hbr.org/webinar/2016/06/the-case-for-bundled-payments-in-health-care
In primary care, about 50%-60% of family physicians are in a capitated model and the rest are in fee for service (FFS). The model is complicated but simplifying things, capitated Doctors earn an amount per patient based on their age and sex to be responsible for their annual healthcare needs. A 16 year old male pays a physician about $70 per year and a 95 year old female pays a physician about $550 per year. In my opinion, the FFS model is backwards because it essentially rewards physicians for being poor physicians (patients come back more frequently) and creates an incentive to physicians to drive patients to their office for things that could be managed through telemedicine, over the phone or email. (Take routine prescription renewals as an example). Besides the physician billings, there is a much greater economic cost associated with this needless visits in patients needing to take time off work to do so, etc, etc.
In the capitated model, if physicians to a “good job” of keeping their patients outside of walk-in clinics, they are given a bonus. However, other than the lost “bonus”, there are no further dis-incentives for a physician to try to keep their patients outside of walk-in clinics. The “double billing” occurs when the MOH is paying a Dr an annual amount to take care of a patients’ annual healthcare needs but that patient may have only seen their Dr once throughout the year and gone to walk-in clinics 20 times. In that case, the MOH pays the capitated Dr their annual “salary” for the patient AND the walk-in clinic Dr’s 20 X $35 (roughly)
This specialist/family doctor contrast is made so often in the press and in Minister Hoskins’ statements. It is inaccurate. Many specialists, including myself, earn no more than family physicians, despite training for many more years. And many specialists have a very high level of overhead expenses.
This is AMAZING! Thank you for breaking down the current and complicated political reality that health care in Canada sometimes is, into a very understandable and well composed summary of the current reality we are facing together. Nothing will be resolved without a system overhaul, and better utilization of all health care human resources – which includes allied health professionals, and not only MDs.